I led a team of students, as part of Stanford Med School’s Disrupt Diabetes design challenge, from problem definition to functioning hardware prototype in 10 weeks winning the design challenge, additional funding and a spot to demo at DiabetesMine 2018.
One Sheet

The Larger Story

Continuous Glucose Monitors (CGM’s) are among the most powerful new technologies improving the quality of life and clinical outcomes for a growing number of people with diabetes.
And yet there are many situations like being in class, on a date, driving in a car, engaged in a meeting doing sports, when loud, repetitive alarms and disruptive screen-watching just don’t work.

Ironically it is often at times when physical or cognitive performance matter most, CGM users have to choose between staying aware of their blood glucose and risking the distraction or embarrassment of a loud alarm calling attention to them among their classmates, colleagues, and friends. Though some customization is available, the current paradigm often leaves CGM users chasing highs and lows and suffering alarm fatigue.
In our survey of over 100 cgm users we found that not one of them had not suffered some negative impacts on their relationships and social life due to CGM alerts, alarms and notifications.
But what if we shifted this vital data stream from audio and visual alerts to the user’s sense of touch? Subtle, ongoing tactile input from your wrist.

Almost imperceptible when you’re steady and in range, but slowly ramping up in intensity and differentiation as you move towards the boundaries of your target numbers.
This would allow you to stay on top of of your blood glucose without even having to look up from a task, or break eye contact with your date, or the road!
This new paradigm of ambient glucose awareness through your sense of touch would enable you to shift your focus back —to what you don’t want to miss.
The research suggests that in as little as 4 days, your brain will, unconsciously learn to recognize the haptic patterns associated with different CGM states and map those to a conscious, sensory awareness of blood glucose. And this happens without conscious effort or additional cognitive load.

After a few days, the patterns will stop feeling like vibration and start feeling like a new sense as your brain begins to sense blood glucose changes through the CGM. Importantly, this would work just as well for parents and caregivers. The sensory augmentation transplants the data stream from the person with diabetes through the CGM, and into the brain of the person wearing our device.
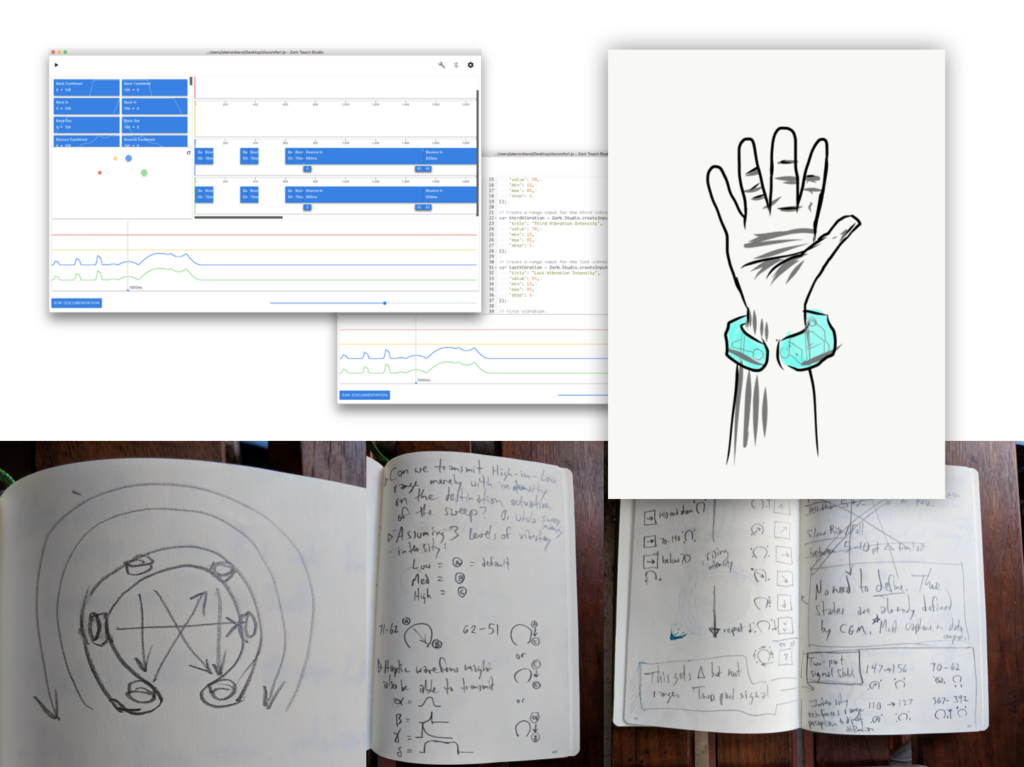
We started sketching prototypes for both haptic hardware and designing haptic patterns that communicate the most common movements of blood glucose.
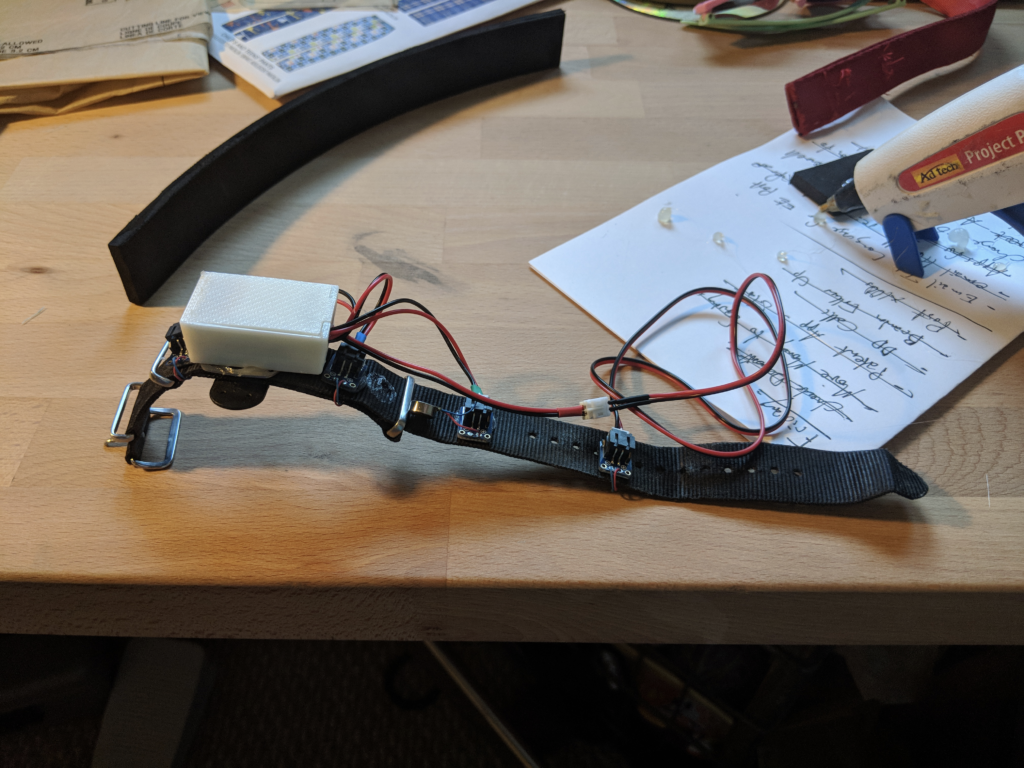
We’ve also been in conversations about partnerships with companies developing hardware for a dedicated haptic device that would serve as the most robust incarnation of bgAWARE.

But hardware takes time. So we are actively developing bgAWARE as an application for the latest Fitbit smartwatches and for the Apple Watch.
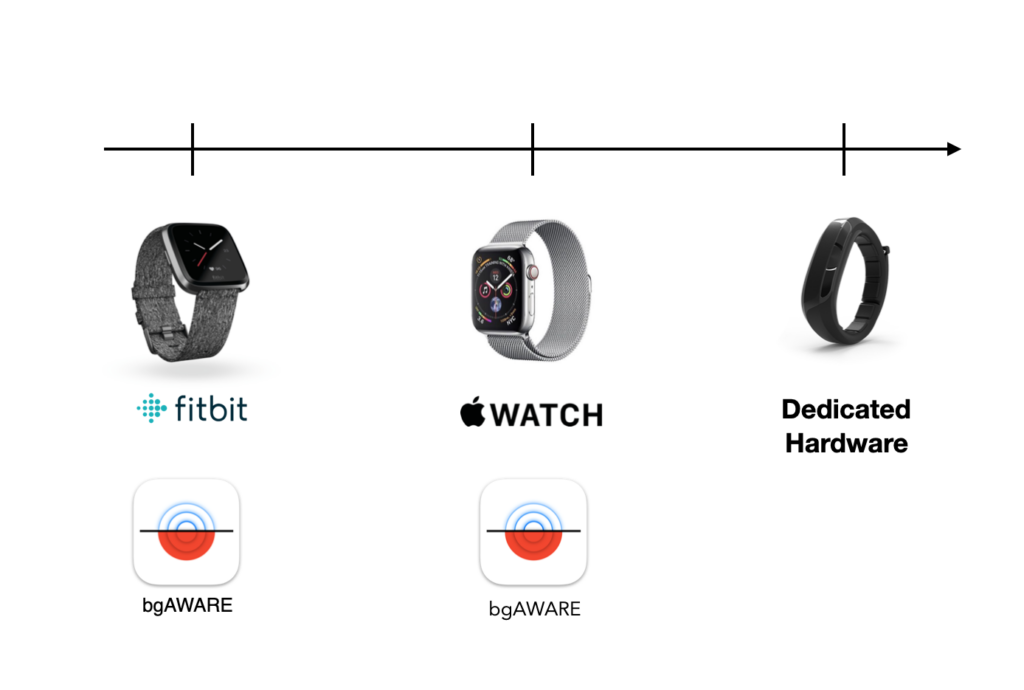
While more limited than the dedicated hardware device we are designing, this will allow us to assess the community interest in a new modality for CGM with existing wearable hardware before we have to the investment needed to get custom hardware to market.

And while some companies are more open with their data than others, we see this as a potentially transformative new interaction model for any CGM pushing an ongoing datastream, including Dexcom, Freestyle Libre with transmitter, and a number of new players about to hit the market promising less-invasive CGM’s.
Epilogue
This pitch won the Disrupt Diabetes Design Challenge, hosted by Stanford Med School and judged by Stanford, Medtronic, IDEO and more.

DiabetesMine 2018 Demo – Full Video
We demo’ed it at DiabetesMine!